12 Diabetic Foot Problems with Pictures
- Last updated on January 4, 2022. Published on
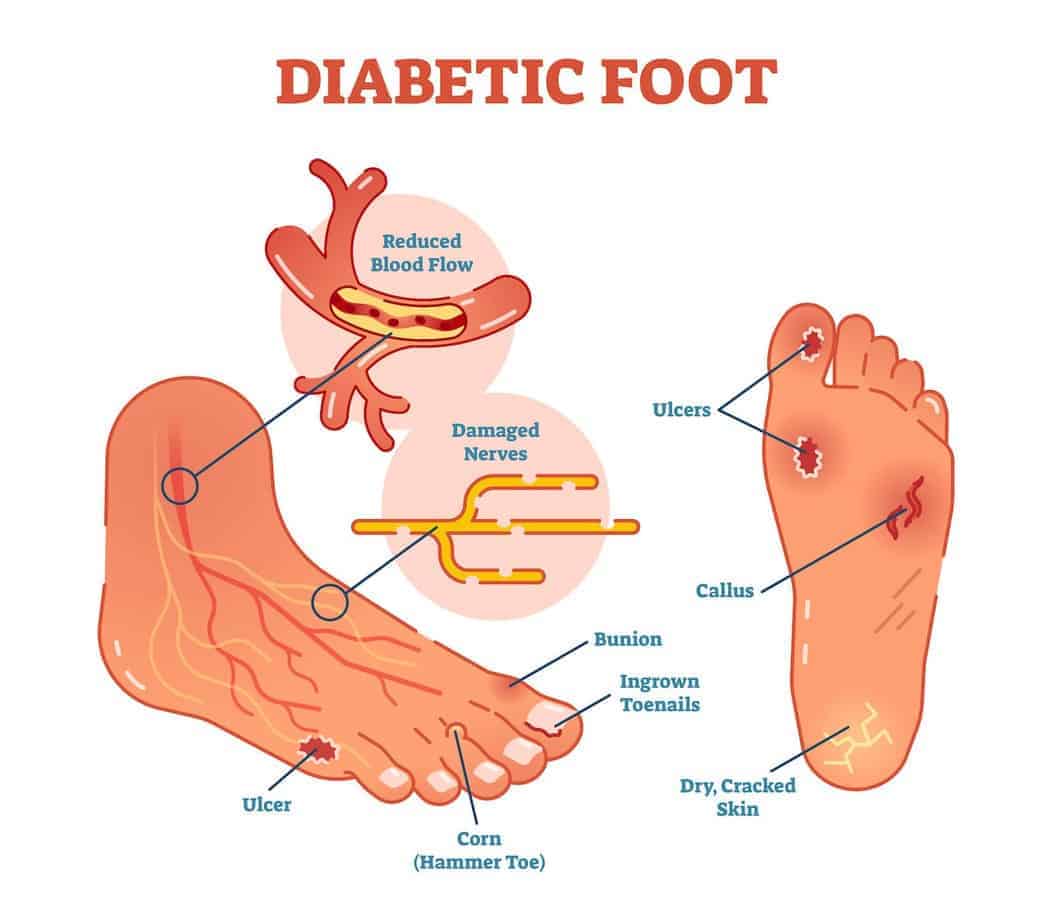
Type 1 and Type 2 diabetes increase the risk of developing foot problems. Peripheral neuropathy and peripheral artery disease, two diabetes complications, can severely affect our feet, causing diabetic foot pain, foot ulcers, blisters, and other problems that can lead to amputations in the worst cases. That’s why people with diabetes must take extra care of their feet and have a diabetic foot exam performed by a health professional at least once a year.
Here are 12 common diabetic foot problems you should be aware of and how to prevent them.
Why do diabetics have foot problems?
Diabetic foot problems are directly linked to diabetes management. If your diabetes is well managed and your glycated hemoglobin (HbA1c) stays below 7%, there is no reason you should develop more foot conditions than the general population.
Foot problems start appearing when diabetes is not managed over a long time. High blood glucose levels can cause severe diabetes complications: diabetic neuropathy and peripheral artery disease. These two conditions are responsible for most diabetes foot problems.
Diabetic Peripheral Neuropathy
Diabetic Neuropathy is nerve damage caused by long-term high blood sugar levels. The most common type of diabetic neuropathy is peripheral neuropathy. It damages the nerves in the body, extremities, feet, legs, and sometimes the hands.
A vast majority of diabetes-related foot conditions come from peripheral neuropathy. When one’s nerves in the feet are damaged, it can be excruciating and sometimes cause a partial or total loss of sensation. This often leads to unnoticed wounds that severely get infected.
Diabetic Peripheral Neuropathy symptoms vary from mild to debilitating and include numbness, reduced ability to feel pain or temperature changes, tingling, burning feet, pain, cramps, increased sensitivity to touch, loss of balance, joint issues, and more.
Diabetic neuropathy also has a significant impact on our muscles and overall balance. Our nerves send and receive electrical messages to control our muscles. When the nerves are damaged, the messages they send and receive are less clear, and our muscles cannot work correctly. That’s why many people with diabetes also suffer from foot alignment problems that can cause deformities such as hammertoes or bunions.
Peripheral Artery Disease
Peripheral artery disease is another diabetes complication that can seriously affect the feet. It reduces the blood flow in our arms and legs, causing a lack of oxygen and nutrients. Wounds take longer to heal, considerably increasing the risks of developing infections, ulcers, or gangrene.
Symptoms of peripheral artery disease vary and can include painful hips and tights, muscle cramps, leg numbness or weakness, cold feet, color change on the legs, loss of hair on lower limbs, slower toenail growth, weaker pulse in legs and feet, and sometimes erectile dysfunction in men.
12 Common Diabetic Foot Problems + Pictures
Here are the 12 most common foot problems you should be concerned about if you have diabetes. Warning: foot problems in people with diabetes can be a sign of severe conditions and lead to serious complications. Always ask for your doctor’s advice and proper diagnosis before taking further steps.
Diabetic (Neuropathy) Foot Pain
Diabetic foot pain is not a foot condition but a symptom of Diabetic Neuropathy. Due to nerves being affected, your feet can become extremely sensitive to pain. The mere contact with the sheet in bed can be unbearable.
Massaging your feet or applying nerve pain relief creams often helps relieve the pain. If you have diabetes and suffer from foot pain, you must seek your doctor’s advice first. Diabetic neuropathy is severe, and you might need medication.
Diabetic Foot Ulcers
Foot ulcers are open sores in the feet that won’t heal long. It generally comes from the breakdown of dry skin and looks like a red crater. Mostly found on the bottom or side of the feet or even on top of a toe.
If the foot nerves are functioning, the ulcer can be very painful. But if not, you may not even notice you have a foot ulcer. Without treatment, a foot ulcer can become infected and lead to severe complications such as a reduced functioning of your foot or even, in some cases, an amputation (6% of people with a diabetic foot ulcer will be hospitalized due to infection or other ulcer-related complication). Nurse Gayle Morris explains how to prevent diabetic foot ulcers.
Warning: foot problems in people with diabetes can be a sign of severe conditions and lead to serious complications. Always ask for your doctor’s advice and proper diagnosis before taking further steps.

Diabetic Blisters
Although blisters are widespread, they can be threatening for people with diabetes due to the higher risks of infection. Diabetic feet are more sensitive and prone to infections. Any blister should be well-taken care of to avoid further complications. Don’t “pop” them: Their upper skin helps prevent a disease!
Blisters are generally caused by friction from your shoes or socks. That’s why diabetic shoes have a seamless and soft protective interior lining, and diabetic socks are crafted in blister-proof materials.
Diabetes Swollen Feet and Ankles
Feet swelling (Edema) is caused by water retention in the feet, ankles, and sometimes legs. It is a common problem among people with diabetes. It can originate from various diabetes-related factors such as poor blood circulation, venous insufficiency, heart or kidney problems, and obesity… Swollen feet can be harrowing and cause great difficulty walking or standing up.
Diabetes Dry Feet and Cracked Heels
High blood sugar levels can cause dehydration, and your skin suffers too. At times, the skin of your feet can get very dry. This is not a “medical condition” but can lead to many. Dry skin can peel or crack and infect, causing further complications such as foot ulcers. An excellent diabetic foot lotion plays a significant role in diabetic foot care.
Dry skin can also be caused by cold. People with diabetes tend to have colder feet than others due to poor blood circulation. To keep your feet warm, consider using one of these thermal diabetic socks.

Athlete's Foot and Toe Nail Fungus
Tinea Pedis – called Athlete’s Foot – is a contagious fungal infection contracted by approximately 20% of the population. It looks like reddish and itchy scales on the skin between the toes and the soles. People with diabetes are at higher risk of Tinea Pedis and other fungus infections of the feet. They often develop more severe complications, sometimes leading to infections, foot ulcers, gangrene, and in extreme cases, amputation. Treatment is often an OTC cream, but ask for your doctor’s advice first.
In case of repetitive fungal infections, consider wearing diabetic socks made with anti-fungal materials such as nano-fibers or bamboo textiles.

Diabetic Foot Calluses and Corns
Both calluses and corns are thicker and more complex layers of skin on the feet or toes. They’re often caused by poorly fitted footwear that causes friction or pressure points on a specific part of your feet. Uneven weight distribution on your feet can also cause calluses and corns. The first step to take is to get adequate shoes that fit correctly.
For most people, they’re temporary and benign. But if you have diabetes, you risk developing complications from calluses and corns. That’s why you should seek your doctor’s advice if they appear.

Toe Deformities caused by Neuropathy
Hammertoe is a deformity of toe joints caused by muscle or tendon imbalance, leading to one or several toes being bent. Diabetic neuropathy weakens feet muscles, making hammertoes and bent toes more common among people with diabetes. They can be very painful at an advanced stage, especially when wearing shoes.
Bunions are progressive deformities of the big toe that angles toward the second toe. It often comes with redness and callused skin. Like hammertoes, it can cause severe pain and sometimes lead to surgery to realign the toes.
When orthopedic shoes are not enough, surgery is sometimes the ultimate treatment.

Ingrown Toenails
Ingrown toenails are a common condition in which the corner or the side of a toenail grows into the flesh. It is not necessarily threatening but can cause extreme pain and high risks of infection. People with diabetes are more at risk of disease from ingrown toenails than others. The most common cause is pressure from the shoes.
Sweaty Feet with Diabetes
Excessive feet sweating can be a big problem for people with diabetes. To avoid bacterial and fungus infections, your feet must stay dry—several medical solutions for extreme foot sweating, such as iontophoresis or even botox injections. But before getting to such heavy treatments, try wearing moisture-wicking socks or using an antiperspirant such as Carpe’s antiperspirant foot lotion. Ask for your doctor’s advice!
Diabetic Foot Gangrene
Gangrene is the death of body tissues due to reduced blood flow or bacterial infection. It commonly starts in body extremities such as the toes. If diagnosed at an early stage, gangrene can be cured. But the prognosis can be terrible if left untreated for a long time (amputation or even death). People with diabetes are at more risk of developing foot gangrene than people without diabetes, mainly because of the prevalence of peripheral artery disease among them.
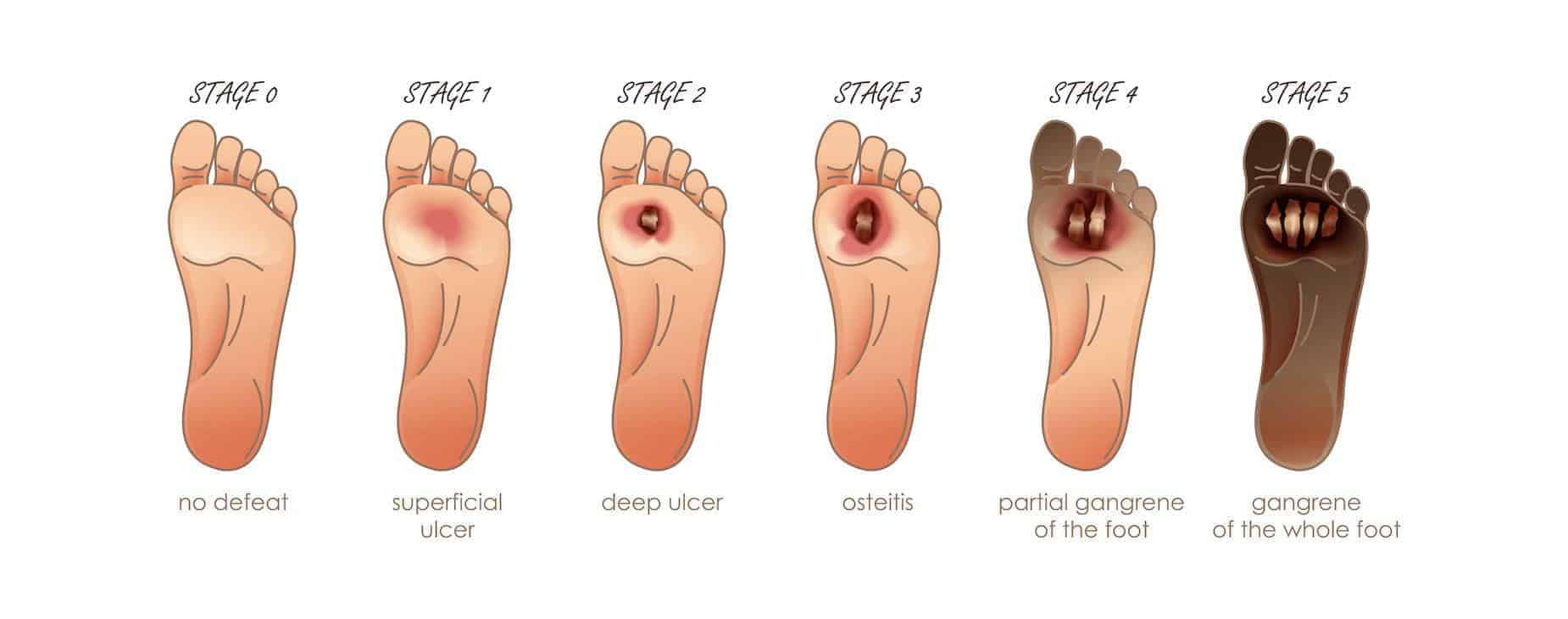
Foot Amputation
Amputation. It’s a word people with diabetes have all heard about, and that frightens us all. And for a good reason: it does happen. If not taken care of, each of the above-mentioned diabetic foot problems can ultimately lead to amputating of a toe, a foot, and sometimes even a leg. Most lower-limb amputations in people with diabetes originate from foot ulcers and gangrene.
- 80% of amputations begin with foot ulcers
- In the USA, 108,000 adults had lower extremity amputations relating to diabetes in 2014 (National Diabetes Statistics Report)
- That equals 5 out of 1000 people living with diabetes
- Of non-traumatic amputations in the US, an estimated 60% are performed on people with diabetes
- Lower limb amputations have gone down by more than 50% in the past 20 years mostly due to better diabetes management
How to Prevent Foot Problems with Diabetes?
First, it’s not because of diabetes that you will necessarily have foot problems. If your blood sugar levels stay in the range and your HbA1c remains below 7%, you should be fine, and there’s no reason you’d have more foot problems than others. Following a strict foot care routine and wearing appropriate shoes also helps prevent most diabetic foot problems and their complications.
Keep your HbA1c below 7%
Diabetic foot problems generally appear after a few years of repetitive “uncontrolled” blood glucose levels. The first and most efficient way to prevent them is to manage your diabetes properly. Keep your blood sugar levels in the range as much as possible and your HbA1c below 7%. Follow your doctor’s advice about nutrition, physical exercise, and medication. If your diabetes is well managed, you should not be at greater risk of developing foot conditions than someone who does not have diabetes.
Inspect your feet daily
Visual inspection of your feet is essential. If you suffer from diabetic neuropathy or peripheral artery disease, the possible decreased sensation in your lower limbs can lead to cuts and wounds staying unnoticed and getting infected.
Check for redness, blisters, black spots, cuts, swelling, bruises, or other suspicious skin modifications or painful areas. If you notice anything unusual, ask for your doctor’s advice before taking further steps.
Follow a diabetic foot care routine
Whether you live with Type 1 or Type 2 diabetes, you must take extra care of your feet. Please wash your feet with non-aggressive cleansing products. Your feet must stay dry and healthy, but your skin must be moisturized enough not to crack. Temperature is also critical, as cold feet get dehydrated, and feet that are too warm are at higher risk of fungal infections. Follow these ten-step diabetic foot care routine that helps you avoid most foot problems.
Get a yearly diabetic foot exam
Everyone with diabetes should get a thorough foot exam from a health professional at least once a year. A diabetic foot exam is a risk-free and painless series of medical tests to identify symptoms of potential diabetes complications (peripheral neuropathy and peripheral artery disease) that could affect your feet.
Medicare covers yearly foot exams if you have diabetes-related nerve damage. Foot exams detect foot problems early and initiate treatments that prevent complications and foot amputation.
Wear diabetic shoes
Most foot problems are caused by poor quality or poorly fitted footwear that hurts your feet. Wearing quality shoes plays a preventive and curative role in diabetic foot.
Foot professionals design diabetic shoes to prevent and address diabetic foot problems. They’re non-binding to boost blood circulation and have a protective seam-free interior that causes no pressure points, frictions, or blisters. Your feet are protected with extra support, padding, and cushioning. The best ones are made with moisture-wicking and breathable materials so your feet stay in a dry and healthy environment.